Pulmonary embolism occurs when a blood clot, usually from the legs, travels to the lungs and blocks a pulmonary artery. This blockage can reduce or stop blood flow to part of the lung, which can damage lung tissue and lead to dangerous complications. The longer the blockage remains untreated, the more severe the pulmonary embolism complications can become.
Understanding how to recognize the symptoms and act quickly can reduce the risk of life-threatening consequences. Let’s explore what a pulmonary embolism is, why it happens, and what can be done to treat and prevent it.
What Is Pulmonary Embolism?
A pulmonary embolism (PE) is a blockage in one of the pulmonary arteries in the lungs, most commonly caused by a blood clot that forms in the deep veins of the legs, known as deep vein thrombosis (DVT). When this clot travels to the lungs, it obstructs blood flow, leading to reduced oxygen levels and stress on the heart.
In simple terms, what is an embolism in the lung? It’s when a blood clot or other material blocks a lung artery, stopping oxygen from reaching your blood. This can have serious implications for your overall health if not treated immediately.
Pulmonary Embolism Causes
The most common cause of pulmonary embolism is deep vein thrombosis (DVT), but there are several other factors that can lead to this condition, including:
- Prolonged immobility: Sitting for long periods, such as during long flights or car rides, can lead to blood clots.
- Surgery: Major surgeries, especially on the legs or abdomen, can increase the risk of developing blood clots.
- Medical conditions: Heart disease, cancer, and some genetic clotting disorders increase the risk of clot formation.
- Injury: Severe trauma, such as bone fractures or muscle injuries, can trigger blood clotting.
By understanding these causes, you can take steps to prevent pulmonary embolism.
Risk Factors
Certain individuals are at a higher risk of developing pulmonary embolism complications due to specific risk factors:
- Age: The risk of PE increases with age, especially after 60.
- Pregnancy: Pregnancy increases pressure on the veins in the pelvis and legs, which may lead to clots.
- Smoking: Smoking damages blood vessels and increases the risk of clot formation.
- Obesity: Excess weight increases pressure in the veins and the risk of clotting.
- Hormonal therapies: Birth control pills and hormone replacement therapy can increase clotting risks.
If you have any of these risk factors, it’s essential to discuss them with your doctor to minimize your chances of pulmonary embolism.
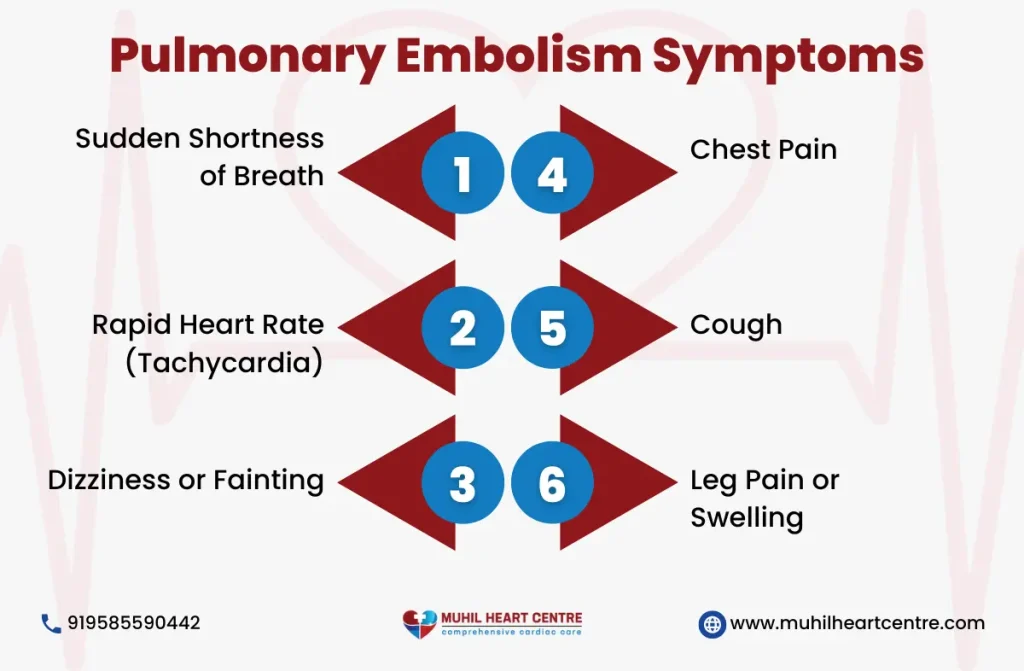
Pulmonary Embolism Symptoms
Recognizing the signs of a pulmonary embolism early can make all the difference. Symptoms can vary but commonly include:
- Shortness of breath: This may occur suddenly and get worse with activity.
- Chest pain: Sharp pain that often feels like a heart attack and gets worse when breathing deeply.
- Coughing: Sometimes accompanied by bloody or blood-streaked mucus.
- Dizziness or lightheadedness: This may indicate a drop in blood pressure.
- Rapid pulse: An abnormally fast heartbeat could signal that your heart is working harder to move blood through blocked arteries.
These symptoms require immediate medical attention to avoid pulmonary embolism complications.
Pulmonary Embolism Complications
Pulmonary embolism complications can be severe and life-threatening if not treated in time. Some of the most common complications include:
- Pulmonary hypertension: Increased pressure in the arteries of the lungs, causing heart strain.
- Heart failure: In severe cases, a PE can cause the right side of the heart to fail due to the increased pressure.
- Lung damage: If the blood flow to the lungs is blocked for too long, parts of the lung tissue can die (infarction).
- Low oxygen levels: This can lead to organ damage or failure, especially in severe cases.
- Recurrence: Without treatment, people who have experienced one pulmonary embolism are at higher risk of having another.
Understanding these pulmonary embolism complications can help emphasize the importance of early diagnosis and treatment.
Pulmonary Embolism Diagnosis Criteria
To diagnose a pulmonary embolism, doctors use a combination of tests and evaluations. Pulmonary embolism diagnosis criteria typically include:
- D-dimer blood test: Measures a substance released when a blood clot dissolves.
- Imaging tests: CT pulmonary angiography or a ventilation-perfusion scan (V/Q scan) to detect blockages.
- Ultrasound: Often used to check for deep vein thrombosis in the legs, which could lead to a PE.
By following these pulmonary embolism diagnosis criteria, healthcare providers can quickly identify the presence of clots and determine the best treatment approach.
What Is the Treatment for Pulmonary Embolism?
So, what is the treatment for pulmonary embolism? Treatment for PE depends on the severity of the condition but generally includes:
- Anticoagulants: Blood thinners that prevent further clotting and allow the body to dissolve existing clots.
- Thrombolytics: Medications that break up clots quickly, typically used in life-threatening cases.
- Surgery: In severe cases, surgery may be required to remove the clot or insert a filter into the large vein to prevent future clots from reaching the lungs.
Each treatment plan is tailored to the individual, depending on their risk factors and severity of the PE. Timely intervention is key to reducing pulmonary embolism complications.
Prevention
Preventing a pulmonary embolism is possible by addressing the risk factors. Here are some tips to help prevent pulmonary embolism complications:
- Stay Active: Move around regularly, especially during long trips or periods of inactivity.
- Stay Hydrated: Drink plenty of water, as dehydration can increase the risk of clots.
- Wear Compression Stockings: These can help prevent blood clots, especially after surgery or during long periods of immobility.
- Quit Smoking: Smoking increases your risk of blood clots, so quitting can significantly reduce your chances of PE.
By taking preventive steps, you can lower your risk of developing pulmonary embolism complications and protect your heart and lungs.
Conclusion
Pulmonary embolism complications are serious and can be life-threatening if not addressed quickly. Understanding the causes, risk factors, symptoms, and treatment options for pulmonary embolism is essential for preventing severe health consequences. If you experience any symptoms of pulmonary embolism, seek medical attention immediately. Early detection and treatment are the best ways to avoid complications. For more information or to schedule a consultation, contact your healthcare provider today.

